The basics
What is Parkinson’s?
Parkinson’s disease (PD) is a neurodegenerative brain disorder that progresses slowly and affects each person differently. One of the greatest challenges of this disease is that it causes both physical and cognitive decline and symptoms. Over time, brain cells produce less and less dopamine, a neurotransmitter that helps control the brain’s reward and pleasure centers and regulate movement and emotional responses.
For most people, symptoms take several years to develop, enabling them to live at home for many more years with the disease.
Non-motor symptoms typically appear first: sleep problems, difficulty concentrating and planning, fatigue, constipation, a reduced ability to smell and detect odors called hyposmia. Mood changes—feeling anxious, irritable, down, or depressed—also can be an early symptom of PD. For most people, these symptoms begin to appear several years before there are any signs of motor symptoms. While Parkinson’s motor symptoms are more widely known, the non-motor symptoms can be far more troublesome and disabling.
Motor symptoms begin to appear when 60 to 80% of the dopamine-producing cells in the brain become damaged and are no longer able produce enough dopamine to relay messages in the brain. As the disease progresses and the brain slowly stops producing dopamine, a person will have a diminishing ability to control their movements, body, and emotions. The four main motor symptoms are tremors, slowness of movement, muscle stiffness, and trouble with balance. A variety of secondary motor symptoms often follow.
Common Parkinson’s motor symptoms.
While symptoms progress differently for everyone, there are common main symptoms.
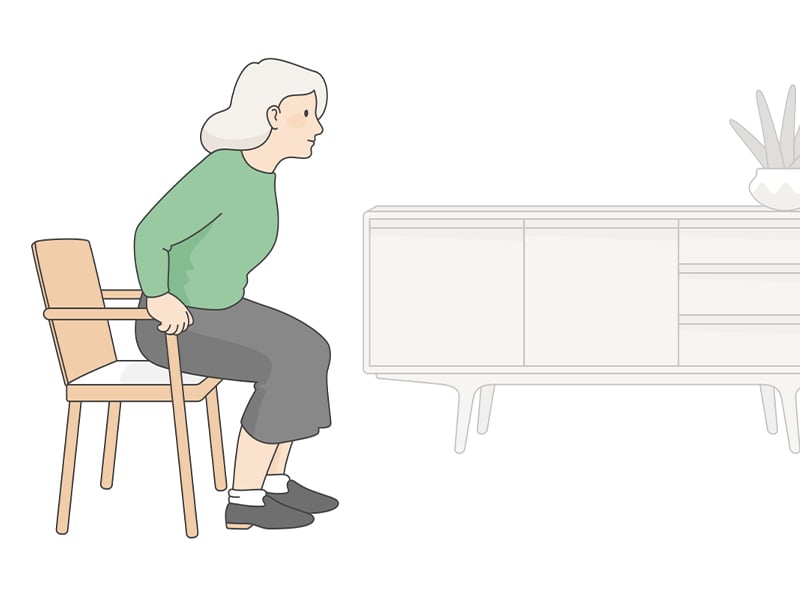
Slowness of movement
Known as bradykinesia, this makes starting and performing physical actions such as getting out of bed, buttoning a shirt, or speaking more difficult.
Involuntary shaking or tremor
A tremor usually occurs in the hand on the affected side but also can appear in other parts of the body.
Muscle stiffness
Muscles in the arms, legs, or torso feel unusually tight, stiff, or achy.
Trouble with balance and falls
This postural instability causes difficulty with balance, walking, and turning around. Frequent falls may occur without explanation.
Freezing
A common phenomenon of being stuck in place when trying to walk or take a step.
Soft or low voice
Called hypophonia, this affects voice volume and can cause muffled speech.
Trouble swallowing
Decreased ability in automatic reflexes such as swallowing and blinking.
If you have been diagnosed with Parkinson’s...
Feel your emotions
You will go through many different emotions as the disease progresses and you face new challenges. Allow yourself to feel and express your emotions in healthy ways.
Educate yourself
Learn as much as possible about the disease and how it will likely affect you and your family as it progresses.
Get involved in your care
Take an active role in your own health and your care plan. Be sure to work with your doctors to optimize your medications.
Communicate directly
Be clear with family members and care providers about your priorities, needs, and wants.
Reach out to others
Spending time with other people who have PD can help you learn about the disease and feel encouraged.
Stay positive
Focus on what you can do rather than what you cannot do. Explore new activities and new ways to find happiness and fulfillment.
While the symptoms and progression of this disease vary from person to person, Parkinson’s is generally defined by five stages, ranging from mild symptoms that don’t interfere with daily activities to advanced severe symptoms that are quite limiting and often debilitating. By Stage Three, most people with Parkinson’s experience loss of balance and trouble controlling their movement. This is when families find that adding a Care Professional to their caregiving team can be helpful.
A home Care Professional can provide respite care for family members and assist the care recipient with dressing, eating, and personal care that may be painful or difficult as well as helping with mobility to stay active and avoid falls. Home care enables people with Parkinson’s to continue to live at home with as much independence as possible while also receiving the support and care they need to be safe.
Family members also benefit—getting the time to take care of their own well-being, connect with friends, relieve stress in healthy ways—knowing their loved one is being cared for by a compassionate, trained professional.
If you’re caring for someone with Parkinson’s…
When someone you love is diagnosed with Parkinson’s, everything changes. Some things change quickly, others change slowly. Be prepared to adapt at every stage, be patient, and pace yourself. If you’re the primary caregiver, you have two equally important responsibilities—to care for your loved one and for yourself.
Don’t help too much
As your loved one’s symptoms progress, you’ll be tempted to help when you see any signs of struggle or frustration. Don’t. Learn to be patient, understand that daily tasks and activities will take longer, and give your loved one plenty of time to do things on their own. With Parkinson’s, maintaining independence and continuing to use muscles and abilities for as long as possible is crucial. Instead of directly helping, focus on creating happiness and comfort—for both of you.
Expect change
Every day will be different. Some days the medication is working fine, then suddenly it seems to stop working, then starts working again. You’ll also notice fluctuating cognition and mood changes. As the disease progresses, your loved one’s ability to feel, think, and evaluate situations and information will become much more challenging. Household roles will change too. With diminishing physical and cognitive abilities, it will be necessary to shift traditional household roles and responsibilities. If you plan for this, these changes will feel more natural and less upsetting.
Be realistic and kind to yourself
If you’re not rested, able to enjoy life, and in good health, you can’t be a good caregiver for your loved one. Be realistic about your needs, physical limitations, and what you can do safely. Make choices that minimize stress and maximize healthy structure, support, and safety for both of you. Also, make time to do the things you enjoy and bring you happiness. And schedule them on your calendar like any other important activity. Remember, you’re living with Parkinson’s—but you’re still living.
Exercise regularly
Exercise is good for all of us. It burns calories, builds muscle, and helps relieve caregiver stress so you feel better and sleep better. For people with Parkinson’s, exercise is vital to maintaining balance, mobility, and the ability to keep doing daily activities. If you’re able to exercise together, set a routine you both can follow—and have fun. Or if you’d rather exercise on your own, do it when your loved one is in physical therapy or taking a Tai Chi or a Dance for Parkinson’s class. Even if you’re feeling tired, make exercise a priority. You’ll stay stronger physically and mentally.
Join (or create) a support group
Making friends with other Parkinson’s caregivers can change your life. You’ll learn from people who have already traveled your path; get new ideas, insights, and encouragement; and find good listeners who can relate to you and your experiences. Inevitably, you will go through many different emotions as you face new challenges. Whether you’re in a formal support group, talking with compassionate friends, or journaling, allow yourself to feel and express your emotions.
Build your knowledge and care team
Continue to read and discover new information on Parkinson’s, techniques to manage the disease, and products that may help your loved one continue to live safely at home. New research is happening all the time. Be sure to stay informed, connected to others, and open about what you need now and may need in the future.
Reaching out for help is far better than hiding out
Determine who you can count on when the going gets tougher—family members, friends, neighbors, Care Professionals—and invite them to join your care team now.
Helpful resources
Visit parkinson.org to learn more about Parkinson’s or to find resources in your area.
Need support? Call the Parkinson Foundation helpline at (800) 473-4636. Nurses, social workers, and therapists are ready to answer questions, provide information, or help you find the local resources you need.
For helpful, inspirational blogs, explore these blogs about Parkinson’s.
Dance for PD offers specialized dance classes for people with Parkinson’s, their families, friends, and care partners. Find a class near you at danceforparkinsons.org.
This information is for educational purposes and is not a substitute for the advice of a medical professional. Source: National Parkinson Foundation.